Written by Emily Locke
Curing HIV/AIDS is still one of the great medical challenges of our time – but now, for the first time, there might be a chance to eradicate the deadly virus worldwide! The start-up company PROVIREX has developed a new technology for genome editing of infected cells, which can be used to remove the genetic material of the pathogen without errors. This innovation offers a tool with which affected patient cells can be permanently and precisely freed from HIV. And where lies the origin of this incredible medical breakthrough? Nowhere other than in Hamburg, Biomol's hometown! A new center for the development of therapies for serious infectious diseases, such as HIV, is now being built here, for which the biotech company PROVIREX is currently establishing special laboratories in Bahrenfeld [1]. This therapy hub will not only enable the further clinical development and economic use of the new genome editing technology, but will also put the Free and Hanseatic City of Hamburg in a leading position in Europe in the field of modern biomedicine!
Subscribe to the free Biomol newsletter and never miss a blog article again!
These topics await you:
1) HIV – A so far Unconquerable Virus
2) From One Virus to Many – The Replication Cycle of HIV
3) The Virus has arrived in the Cell – What now?
4) The usually Fatal Course of an HIV Infection
5) The Pitfalls of Fighting the HI Virus
6) A Glimpse of Hope: New Genome-editing Technology from Hamburg
7) The next Steps on the long and winding Road to an HIV Cure
HIV – A so far Unconquerable Virus
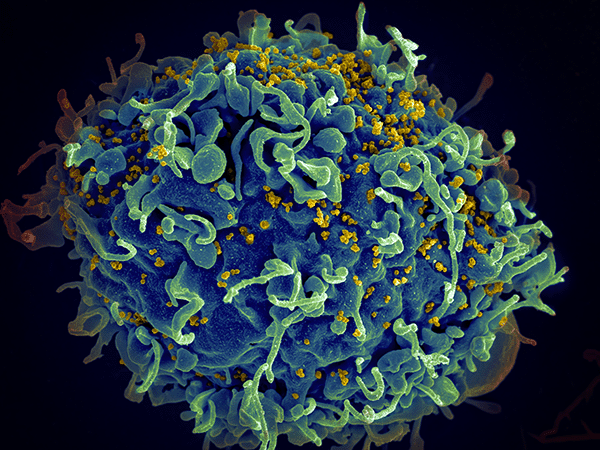
"The deadly plague AIDS" – that was the headline published by SPIEGEL in June 1983. But even today, the human immunodeficiency virus (HIV) continues to claim thousands of lives. In 2021 alone, 38.4 million people were living with HIV, of whom 650,000 eventually died of AIDS, the acquired immunodeficiency syndrome caused by the HI virus [2]. The pathogen is transmitted through contact with body fluids such as blood, semen, vaginal secretions, and breast milk, with the most common route of infection being anal or vaginal intercourse without the use of condoms. Other common routes of infection represent the use of contaminated syringes during intravenous drug use and transmission to the child by an HIV-infected mother during pregnancy or breastfeeding [3].
HIV belongs to the retrovirus family. Two different species of enveloped viruses are known: HIV type I and type II. A virion has a diameter of about 100 to 120 nm, which is larger than average for a virus. The capsid contains the enzymes and accessory proteins that are essential for the survival of the virus particle. Reverse transcriptase, integrase and protease are particularly important for the replication cycle (see Fig. 1) [4].
From One Virus to Many – The Replication Cycle of HIV
In principle, HIV replicates like any other retrovirus – but the special feature of this pathogen lies in the type of cells it infects. Namely, the virus requires host cells that express the CD4 receptor on their surface (CD4+ cells) to replicate. Any immunologist will know that these particularly include the T helper cells. These assist other white blood cells in important immunobiological processes, such as activation of cytotoxic T lymphocytes and maturation of B lymphocytes into plasma and memory cells. Infected, resting CD4+ cells are the reason why HIV has not yet been eradicated and why relapses often occur after discontinuation of therapy with antiretroviral drugs.
HIV, like any other virus, can only replicate with the help of a host. To do this, the viral envelope first fuses with the cell to be infected. This occurs via the binding of the viral surface proteins GP41 and GP120 to the CD4 receptors of the host, after which a conformational change occurs in the transmembrane protein GP41. This process, often referred to as the "snap-action mechanism," fuses the viral and cellular membranes together, thereby allowing the release of genetic information as well as HI virus proteins into the cytoplasm (Fig. 1) [5]. In addition to the CD4 receptor, there are other co-receptors involved in the binding of the virus: the chemokine receptors CCR5 and CXCR4. Differences in the expression of these receptors influence the probability of infection as well as the course of HIV infection [6].

Figure 1: Replication cycle of HIV. Binding to the host cell represents the first step of infection. It involves, among other components, the gp120 envelope protein of the HI-virus. The virus enters the cell through clathrin-mediated endocytosis, where it releases its viral RNA. By the virus's own reverse transcriptase the RNA is transcribed into cDNA, which is then integrated into the host genome. With the use of the protein biosynthesis machinery of the host cell, new virus particles are produced and new viruses are assembled. The final step is the release of the new viruses (Source: https://commons.wikimedia.org/wiki/File:HIV-replication-cycle-en.svg).
The Virus has arrived in the Cell – What now?
Now the HI virus has entered the host cell – but how does it replicate? In order to do this, it first has to complete a rather difficult task: It must integrate its genetic material into that of the host cell. What makes this particularly tricky is that the pathogen has an RNA genome, whereas the genome of the cell exists as double-stranded DNA in the cell nucleus. But even such a significant difference does not seem to be a major hurdle for the HI virus: After all, it brings along the enzyme reverse transcriptase for this purpose. In the cytoplasm of the host cell, this enzyme converts the viral RNA into proviral DNA – a process known as reverse transcription (Fig. 1).
The viral genome is now transported in its DNA form into the cell nucleus, where it is incorporated into the human genome with the help of another enzyme, called integrase [7]. Here, it can now be transcribed by the polymerase of the host cell and subsequently be translated. The resulting precursor proteins are cleaved by the viral protease and then assembled into new virus particles. The mature daughter virions bud off from the plasma membrane and are ready to infect the next cell (Fig. 1).
The usually Fatal Course of an HIV Infection
In this way, the virus spreads further and further through the body – but what is the actual course of a typical infection? First, an acute infection usually occurs after an incubation period of about three to six weeks (Fig. 2). This is accompanied by symptoms such as fever, fatigue and headache – thus, infected persons feel similar to a flu-like infection [8]. This is also the reason why acute HIV infections unfortunately usually remain undetected.
The resulting lack of treatment causes the infection to move into the latent phase. This usually lasts for several years and is not accompanied by serious physical symptoms. Nevertheless, the body's CD4+ T helper cells are continuously destroyed, weakening the immune system. At the same time, the number of copies of viral RNA continuously increases. Non-treatment of the infection leads to a further serious drop in the number of CD4+ cells and a massive increase in the amount of viral RNA. The course eventually ends in a severe immunodeficiency, which is then referred to as AIDS (Fig. 2). This can lead to opportunistic diseases, Kaposi's sarcoma, malignant lymphomas and usually ultimately to the death of the patient [9].

Figure 2: Course of a typical HIV infection. After infection with the HI virus, the number of CD4+ T helper cells decreases sharply. The first phase of the infection is called the acute phase (primary infection), during which the viral load also reaches the first peak. After about nine weeks, the latency period begins, which lasts several years and is usually without serious symptoms. Due to the continuous destruction of T cells and the steady increase in viral particles, the infection finally enters the last phase, the symptoms of which are then summarized as AIDS (Source: https://commons.wikimedia.org/wiki/File:Hiv-timecourse_copy.svg).
The Pitfalls of Fighting the HI Virus
A cure for HIV has not yet been found. Nevertheless, there are so-called antiretroviral therapies (ART) and highly active antiretroviral therapies (HAART), which, through a combination of different drugs, are at least able to slow down the multiplication of the virus in the body and almost completely prevent the outbreak of AIDS. But why is it so difficult to combat HIV? After all, there are effective drugs or even vaccines for all sorts of other (viral) diseases.
The main problem is the fact that the HI virus infects the cells of the immune system. While the body actually wants to defend itself against another pathogen, the infected immune cells instead begin to produce viral proteins and release new viruses. In this way, the virus cleverly evades attack from antiviral drugs and the immune system. Another crucial aspect that complicates the development of effective drugs and vaccines is the unusual survivability of HIV, which results from a high mutation rate. This arises from the extremely error-prone process of reverse transcription, which causes repeated changes in the genetic material [10]. The resulting frequent mutations of surface proteins make it difficult for medicine to combat the virus with antiretroviral drugs or vaccines, thus giving HIV an evolutionary advantage. To put this into perspective, not even half as many new variants of the influenza viruses evolve in the same time in the entire world as of the HI virus in a single, infected human [4].
A Glimpse of Hope: New Genome-editing Technology from Hamburg
However, after many decades of research, the goal may finally have been reached: A cure for HIV and AIDS is in sight. The start-up PROVIREX, which is based in Hamburg, has developed a new technology that could succeed in permanently and precisely ridding infected cells of HIV. It is based on research by Prof. Joachim Hauber at the Leibniz Institute for Experimental Virology, also based in Hamburg, and Prof. Frank Buchholz at the Technical University of Dresden. The principle of the innovative therapeutic approach is based on a site-specific genome surgery technology to precisely excise chromosomally integrated viral genomes, so-called proviruses, using "gene scissors" (Fig. 3) [11].
This gene scissor is a highly specific designer recombinase called Brec1 (Broad Range Recombinase 1). The recombinase recognizes an asymmetric, 34 base pairs long gene sequence found in the LTRs (long terminal repeats) of a majority of clinically relevant HIV type I strains and subtypes. Unlike other segments of the HIV-I genome, this sequence appears to be highly conserved and therefore less susceptible to mutation [12]. An advantage over already established genome editing technologies, such as CRISPR-Cas, is that Brec1 functions independently of host DNA repair. DNA double-strand breaks caused by CRISPR-Cas must be reassembled via homologous repair or non-homologous end-joining. This is not the case with Brec1: the recombinase reassembles the genome of infected cells correctly on its own after removal of proviral HIV DNA and does not cause mutations (Fig. 3). It acts with nucleotide precision and produces completely error-free recombinants! In addition, Brec1 features high specificity and shows unparalleled and durable antiviral effects in vitro and in vivo. PROVIREX confirms that the viral load in plasma decreases to levels below the detection limits of the most sensitive test systems and, moreover, no relapse is observed [13].

Figure 3: The therapeutic mechanism of Brec1. HIV DNA integrated into the host cell genome (proviral DNA) is flanked by LTRs. Brec1 recognizes a specific gene sequence that occurs in the LTRs of numerous HIV types. This allows the recombinase to selectively remove the proviral DNA and also to reassemble the DNA double-strand break independently and without error. The excised viral DNA is then degraded (Source: https://www.provirex.de/).
This short video from the Leibniz Institute for Experimental Virology illustrates the mechanism of Brec1 recombinase: Working Principle of the BREC1 Recombinase
The next Steps on the long and winding Road to an HIV Cure
The innovative technology is not yet in use because, as with any new therapeutic approach, a number of clinical trials must first be completed before the new technology is launched on the market. However, in cooperation with the University Medical Center Hamburg-Eppendorf (UKE), the approach is already being prepared for clinical trials. Initially, it will be evaluated in the context of a stem cell therapy in eight HIV patients at the Clinic for Stem Cell Therapy of the UKE under the direction of Nicolaus Kröger. Corresponding funding and investment have already been provided by the German Federal Ministry of Education and Research (BMBF), the Hamburg Senate and ForTra gGmbH for Research Transfer of the Else Kröner-Fresenius Foundation [11]. In addition, PROVIREX is simultaneously developing new administration forms of desginer recombinases, which should allow easier and direct application by injection [1].
But it does not end with HIV: The new recombinase-based genome editing is a platform technology that is of interest for many other application areas and could simplify numerous other treatments. PROVIREX will continue to work on first-in-class advanced therapy medicinal products (ATMPs) in the future, hopefully enabling the fight against more life-threatening, persistent viral infections [12]. But for now, here at Biomol, we continue to eagerly follow the medically and socially historic breakthrough on the long and winding road to a cure for HIV and AIDS - made in Hamburg!
Special thanks to PROVIREX for permission to use the image as well as the video on Brec1 functionality.
Sources
[1] https://www.hamburg.de/bwfgb/16615938/grundsteinlegung-campus-schlueterstrasse/, last access: 17.11.2022
[2] https://www.unaids.org/en, last access: 17.11.2022
[3] https://www.cdc.gov/hiv/risk/estimates/riskbehaviors.html, last access: 17.11.2022
[4] https://de.wikipedia.org/wiki/HIV, last access: 17.11.2022
[5] Wilen, C. B., Tilton, J. C., Doms, R. W. HIV: cell binding and entry. Cold Spring Harbor perspectives in medicine vol 2,8 (2012).
[6] Winkler, C. et al. Genetic restriction of AIDS pathogenesis by an SDF-1 chemokine gene variant. ALIVE Study, Hemophilia Growth and Development Study (HGDS), Multicenter AIDS Cohort Study (MACS), Multicenter Hemophilia Cohort Study (MHCS), San Francisco City Cohort (SFCC). Science 279(5349):389-93 (1998).
[7] V. Poletti, F. Mavilio. Interactions between Retroviruses and the Host Cell Genome. Molecular therapy. Methods & clinical development vol 8, 31–41 (2018).
[8] Schafberger, A., Sweers, H. HIV / AIDS – Heutiger Wissensstand. Deutsche AIDS-Hilfe e. V. (2008).
[9] https://www.aidshilfe.de/hiv-symptome-verlauf, last access: 17.11.2022
[10] Korber, B. et al. Evolutionary and immunological implications of contemporary HIV-1 variation, British Medical Bulletin, vol 58,1:19–42 (2001).
[11] https://www.bionity.com/de/news/1166076/neuer-ansatz-zur-heilung-von-hiv.html, last access: 17.11.2022
[12] Karpinski, J et al. Directed evolution of a recombinase that excises the provirus of most HIV-1 primary isolates with high specificity. Nat Biotechnol 34, 401–409 (2016).
[13] https://www.provirex.de/, last access: 17.11.2022
Preview image: https://unsplash.com/photos/cI8T6zeDbZw